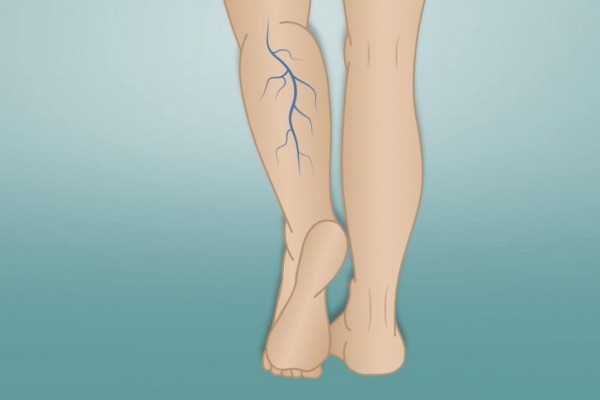
Saphenous vein insufficiency is the most common chronic venous incompetence of lower limbs. It affects more than 30% of adults. The first-line treatment of venous incompetence is thermal ablation, e.g., radiofrequency ablation (RFA) and endovenous laser ablation (EVLA). However, the use of heat energy in thermal ablation was associated with complications such as nerve injury and skin burns.
To avoid thermal energy complications, few novel treatments such as sclerotherapy, cyanoacrylate, and mechanochemical ablation (MOCA) have been introduced. One of MOCA device is ClariVein that combines mechanical injury to the venous endothelium using a rotating wire with simultaneous delivery and dispersion of a liquid sclerosant. The liquid sclerosant causes irreversible damage to the cellular membranes of the endothelium, resulting in the fibrosis of veins. A previous meta-analysis has conducted nonrandomized trials for MOCA. It is important to study the use of MOCA since medium-term follow-up data on randomized clinical trials are now becoming available. Therefore, we performed a meta-analysis of randomized trials aiming to assess the safety and efficacy of MOCA by comparing thermal ablation for saphenous vein insufficiency.
Four studies were finally included in our meta-analysis. The MOCA group had 93.4% of anatomical success rate, whereas the thermal ablation group had 95.8% (1-month follow-up) and 84.5% (more than 6 months to less than a year), whereas the thermal ablation group had 95.8% (1 month follow-up) and 94.8% (more than 6 months to less than a year). There were similar anatomical successes in the MOCA and thermal ablation groups at the 1-month follow-up. The estimated effect of MOCA on anatomical success showed a statistically significant reduction at the mid-term follow-up. MOCA had a lower risk of (DVT, nerve injury, and skin burns than thermal ablation.
Previous meta-analyses that included nonrandomized trials demonstrated that MOCA could be considered an effective treatment for saphenous vein insufficiency; however, these results were based on a pooled analysis of low-quality data. In previous studies, the pooled anatomical success rate at the mid-term follow-up was 91%, 97.1%, and 98.5% for MOCA, RFA, and EVLA, respectively; the rates obtained in our study were lower: 84.5% for MOCA and 94.8% for thermal ablation. Blinding to the assessor may have contributed to the lower anatomical success rate observed in our study.
The major benefit of MOCA reported in previous reviews was pain intensity reduction during the procedure [17, 18]. However, we did not perform an analysis of pain intensity because there was a high risk of measurement bias from no participant blinding in the available trials. The potential benefits in reducing the risk of nerve injury might be of considerable clinical importance for MOCA. The major benefit of MOCA reported in previous reviews was pain intensity reduction during the procedure. However, we did not perform an analysis of pain intensity because there was a high risk of measurement bias from no participant blinding in the available trials. The potential benefits in reducing the risk of nerve injury might be of considerable clinical importance for MOCA. Our meta-analysis indicated that MOCA had a lower risk of major complications compared with thermal ablation. Nerve injury was seen in 0.4% and 3.2% cases after MOCA and thermal ablation, respectively.
Author: Johanes Nugroho
Full article available at: https://www.hindawi.com/journals/ijvm/2020/8758905/